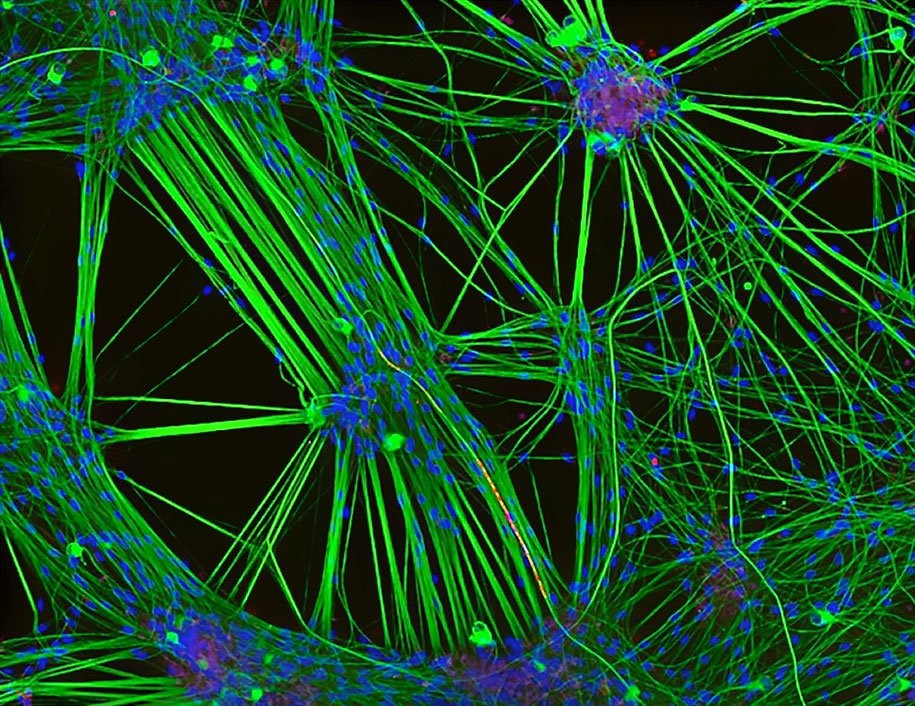
Cultivo de neuronas (teñido de verde) procedentes de células de piel humana y células de Schwann, un segundo tipo de célula cerebral (teñido de rojo). (Foto: Rebecca Nutbrown/Nikon Small World 2016)
La estimulación del Vago, en una serie de procesos difíciles de tratar con otras técnicas, nos ha llenado de esperanza.
En la epilepsia , artritis reumatoide, cefaleas, insuficiencia cardiaca y depresión, esta técnica se ha mostrado desde hace ya un cuarto de siglo. Es simple, eficaz, barata y con complicaciones soportables.
No obstante, creo que se puede simlificar y saobre trodo encontrar como el sistema vegetativo y concretamente el polivagal, regula varios procesos patalogicos
Journal of Neurosurgery
Dec 2011 / Vol. 115 / No. 6 / Pages 1248-1255
Vagus nerve stimulation for epilepsy: a meta-analysis of efficacy and predictors of response
A review Dario J. Englot, M.D., Ph.D., Edward F. Chang, M.D., and Kurtis I. Auguste, M.D.
Department of Neurological Surgery, University of California, San Francisco, California
Abbreviations used in this paper: HSD = honestly significant difference; LSD = least significant difference; VNS = vagus nerve stimulation.
Vagus nerve stimulation (VNS) was approved by the US FDA in 1997 as an adjunctive treatment for medically refractory epilepsy. It is considered for use in patients who are poor candidates for resection or those in whom resection has failed. However, disagreement regarding the utility of VNS in epilepsy continues because of the variability in benefit reported across clinical studies. Moreover, although VNS was approved only for adults and adolescents with partial epilepsy, its efficacy in children and in patients with generalized epilepsy remains unclear. The authors performed the first meta-analysis of VNS efficacy in epilepsy, identifying 74 clinical studies with 3321 patients suffering from intractable epilepsy. These studies included 3 blinded, randomized controlled trials (Class I evidence); 2 nonblinded, randomized controlled trials (Class II evidence); 10 prospective studies (Class III evidence); and numerous retrospective studies. After VNS, seizure frequency was reduced by an average of 45%, with a 36% reduction in seizures at 3–12 months after surgery and a 51% reduction after > 1 year of therapy. At the last follow-up, seizures were reduced by 50% or more in approximately 50% of the patients, and VNS predicted a ≥ 50% reduction in seizures with a main effects OR of 1.83 (95% CI 1.80–1.86). Patients with generalized epilepsy and children benefited significantly from VNS despite their exclusion from initial approval of the device. Furthermore, posttraumatic epilepsy and tuberous sclerosis were positive predictors of a favorable outcome. In conclusion, VNS is an effective and relatively safe adjunctive therapy in patients with medically refractory epilepsy not amenable to resection. However, it is important to recognize that complete seizure freedom is rarely achieved using VNS and that a quarter of patients do not receive any benefit from therapy.
•
The New England Journal of Medicine
Early Identification of Refractory Epilepsy
Patrick Kwan, M.D., and Martin J. Brodie, M.D.N Engl J Med 2000; 342:314-319 February 3, 2000DOI: 10.1056/NEJM200002033420503
Share:
Epilepsy is estimated to affect approximately 50 million people worldwide.1 Although the prognosis for the majority of patients is good,2 up to 30 percent do not have remission despite appropriate therapy with antiepileptic drugs3-5; the results are substantial deleterious effects on individual health and quality of life and a heavy burden on society.6 The characteristics of this group of patients are ill defined, but possible unfavorable prognostic factors include an early onset of epilepsy and the presence of symptomatic or cryptogenic epilepsy, multiple types of seizures, large numbers of seizures before treatment, complex febrile seizures or febrile status epilepticus, and generalized epileptiform activity on surface electroencephalography.7,8 In the 1990s, eight new antiepileptic drugs were licensed worldwide,9 some of which are now available for monotherapy. We conducted a prospective observational study of patients who were given a diagnosis of epilepsy, treated, and followed up at a single center in which we evaluated their response to antiepileptic-drug therapy and attempted to determine the factors associated with a poor response to therapy
Neurosurgery:
December 2000 – Volume 47 – Issue 6 – pp 1353-1358
Clinical Studies
Efficacy of Vagal Nerve Stimulation in Children with Medically Refractory Epilepsy
Patwardhan, Ravish V. M.D.; Stong, Benjamin B.A.; Bebin, E. Martina M.D.; Mathisen, Jan M.D.; Grabb, Paul A. M.D.
Abstract
OBJECTIVE: The effects of vagal nerve stimulation (VNS) on seizure frequency and quality of life were analyzed retrospectively in children with medically refractory epilepsy.
METHODS: Thirty-eight children aged 11 months to 16 years underwent implantation of vagal nerve stimulators. Age of seizure onset, duration of epilepsy, and seizure type and frequency were recorded preoperatively. Age at implantation, length of follow-up, seizure type and frequency, and change in quality of life (QOL) were recorded postoperatively. Changes in QOL were assigned a QOL score by the caretakers on a visual analog scale of −1 (much worse) to +1 (much improved).
RESULTS: The median follow-up period was 12 months (range, 10–18 mo). Eleven (29%), 15 (39%), 5 (13%), and 7 (18%) children had greater than 90% reduction, 50 to 90% reduction, less than 50% reduction, and no reduction in seizure frequency, respectively. For all children, seizure reduction by seizure type was as follows: atonic (80%), absence (65%), complex partial (48%), and generalized tonicoclonic (45%). The mean change in QOL score was 0.61. Eighty-six percent of the children had QOL scores of 0.5 (improved) or higher. Follow-up of at least 6 months was associated with greater seizure reduction (P = 0.05) and higher QOL score (P < 0.01). Seizure reduction was greater in children with onset of epilepsy after 1 year of age (P < 0.05). The age of the child and duration of epilepsy were not associated with greater or lesser degrees of seizure reduction.
CONCLUSION: VNS provided improvements in seizure control for the majority of children regardless of age. QOL was improved in the majority of children with VNS. VNS should be considered for children with medically refractory epilepsy who have no surgically resectable focus.
Journal of Neurosurgery
May 1989 / Vol. 70 / No. 5 / Pages 667-675
CLINICAL ARTICLES
Electrophysiological connections between the hippocampus and entorhinal cortex in patients with complex partial seizures
• Paul A. Rutecki, M.D.,
• Robert G. Grossman, M.D.,
• Dawna Armstrong, M.D., and
• Susan Irish-Loewen,R.E.E.G.T.
Departments of Neurology (Section of Neurophysiology), Neurosurgery, and Pathology, Baylor College of Medicine, Houston, Texas
Address reprint requests to: Robert G. Grossman, M.D., Department of Neurosurgery, Baylor College of Medicine, One Baylor Plaza, Houston, Texas 77030.
Dr. Rutecki was supported in part by Clinical Investigator Development Award NS01049 from the National Institutes of Health and an Esther A. and Joseph Klingenstein Fellowship in the Neurosciences.
Related Articles
By Keywords:
complex partial seizures, Ammon's horn sclerosis, epilepsy, hippocampus, entorhinal cortex, evoked responses
Abstract
✓ The electrophysiological properties of the neural pathways between the hippocampus and the entorhinal cortex were studied intraoperatively in 31 patients undergoing anterior temporal lobectomy for medically intractable complex partial seizures. The hippocampus, removed en bloc, was studied histologically and the pathology was correlated with the electrophysiological findings. In 29 of the patients, entorhinal stimulation evoked a characteristic positive-negative potential in the hippocampus. The entorhinal-evoked hippocampal response closely resembled, or was identical to, the spontaneously occurring hippocampal interictal spike discharge. In patients with Ammon's horn sclerosis in whom there was a major loss of neurons in the hippocampal subfields CA1, CA3, and CA4, the evoked responses were of simple morphology and long latency(mean 21.9 msec to the peak of the first potential). In patients with a ganglioglioma in whom the hippocampus was histologically normal, the evoked responses were of greater complexity and shorter latency (mean 11.8 msec). Stimulation at a single entorhinal site evoked similar waveforms at different hippocampal recording sites. Conversely, stimulation at different entorhinal sites evoked similar responses at a single hippocampal recording site. Stimulation of the hippocampus evoked a potential in the entorhinal cortex and, in some instances, in the amygdala, insula, and lateral temporal cortex. These connections may produce a positive feedback loop that favors seizure generation.
J Korean Med Sci. 2007 Jun;22(3):442-445. English.
Published online June 30, 2007. https://doi.org/10.3346/jkms.2007.22.3.442
Copyright © 2007 The Korean Academy of Medical Sciences
Vagus Nerve Stimulation in Intractable Childhood Epilepsy: a Korean Multicenter Experience
Su Jeong You, Hoon-Chul Kang, Heung Dong Kim,* Tae-Sung Ko, † Deok-Soo Kim,‡ Yong Soon Hwang,§Dong Suk Kim,∥ Jung-Kyo Lee,¶ and Sang Keun Park§
Department of Pediatrics, Epilepsy Center, Inje University College of Medicine, Sanggye Paik Hospital, Seoul, Korea.
*Department of Pediatrics, Pediatric Epilepsy Clinics, Severance Child's Hospital, Brain Research Institute, Yonsei University College of Medicine, Seoul, Korea.
†Department of Pediatrics, Asan Medical Center, Ulsan University College of Medicine, Seoul, Korea.
‡Department of Pediatrics, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
§Department of Neurosurgery, Epilepsy Center, Inje University College of Medicine, Sang-gye Paik Hospital, Seoul, Korea.
∥Department of Neurosurgery, Severance Hospital, Handicapped Children's Research Institute, Brain Research Institute, Yonsei University College of Medicine, Seoul, Korea.
¶Department of Neurosurgery, Ulsan University College of Medicine, Asan Medical Center, Seoul, Korea.
Received July 12, 2006; Accepted October 10, 2006.
We evaluated the long-term outcome of vagus nerve stimulation (VNS) in 28 children with refractory epilepsy. Of these 28 children, 15 (53.6%) showed a >50% reduction in seizure frequency and 9 (32.1%) had a >75% reduction. When we compared seizure reduction rates according to seizure types (generalized vs. partial) and etiologies (symptomatic vs. cryptogenic), we found no significant differences. In addition, there was no correlation between the length of the stimulation period and treatment effect. The seizure reduction rate, however, tended to be inversely related to the seizure duration before VNS implantation and age at the time of VNS therapy. VNS also improved quality of life in this group of patients, including improved memory in 9 (32.1%), improved mood in 12 (42.9%), improved behavior in 11 (39.3%), improved altertness in 12 (42.9%), improved achievement in 6 (21.4%), and improved verbal skills in 8 (28.6%). Adverse events included hoarseness in 7 patients, dyspnea at sleep in 2 patients, and wound infection in 1 patient, but all were transient and successfully managed by careful follow-up and adjustment of parameters. These results indicate that VNS is a safe and effective alternative therapy for pediatric refractory epilepsy, without significant adverse events.
RESULTADOS DE LA ESTIMULACIÓN DEL NERVIO VAGO EN PACIENTES CON EPILEPSIA FARMACORRESISTENTE EN UN CENTRO DE REFERENCIA NACIONAL DE EPILEPSIA
Pedro Roldán-Ramos, Luis A. Reyes-Figueroa, Jordi Rumià, Eva Martínez-Lizana, Antonio Donaire, Mar Carreño-Martínez
Objetivos. Describir los resultados clínicos y complicaciones derivados de la estimulación vagal en pacientes con epilepsia farmacorresistente no tributaria de otras modalidades de tratamiento quirúrgico, desde el primer implante en un centro de referencia nacional.
Pacientes y métodos. Se realizó un análisis retrospectivo de los pacientes implantados en nuestro centro y se extrajeron datos relativos a las características basales de su epilepsia y complicaciones derivadas.
Resultados. Se incluyeron 32 nuevos implantes en 31 pacientes, con una edad media de 34 años, evolución de enfermedad de 29,3 años, tres fármacos antiepilépticos prequirúrgicos y 4,03 años de seguimiento. Las crisis parciales complejas (71,9%) y criptogénicas (59,4%) fueron el tipo y la etiología de crisis más frecuentes. El 75% no tenía antecedentes quirúrgicos de epilepsia. Un 43,8% presentó mejoría igual o superior al 50%, mayor en las epilepsias parciales complejas (p = 0,22) y la etiología criptogénica. No se halló asociación estadística entre ajustes de medicación y frecuencia de las crisis. Los efectos secundarios encontrados fueron disfonía, ronquera y disfagia transitorias, y una asistolia intraoperatoria recuperada. Se realizó un recambio por ruptura de hardware postraumática. Un paciente con paresia preexistente de cuerda vocal presentó estridor laríngeo que requirió ajuste de intensidad, y se produjo una retirada del sistema por disfunción. En el 84,4%, la tolerancia fue excelente.
Conclusiones. Constituye un tratamiento efectivo para mejorar significativamente la frecuencia de crisis de los pacientes farmacorresistentes y con contraindicación para otras modalidades de tratamiento quirúrgico. Se precisan futuros estudios para predecir la respuesta individual de cada paciente, optimizar las indicaciones y mejorar la relación coste/beneficio.